MDX Hawaii is pleased to announce it has executed an agreement with Conifer Health Solutions (Conifer) to provide MSO services for MDX’s Medicare line of business effective for dates of service January 1, 2024 and after.
Important Update: New Policy for Referrals to Specialists for Humana HMO Members
Aloha MDX Providers,
As part of our ongoing effort to streamline access to care and reduce administrative burden, we are very pleased to inform you of an important update to our specialty referral policy.
Effective 7/16/25, you no longer need to submit Specialty Referral forms for Humana HMO members receiving care from in-network specialists.
- Specialty Referral is still required for a referral of a Humana HMO member to an out-of-network specialist.
- Failure to obtain prior approval for services rendered by an out-of-network provider will result in a claim denial.
- Prior Authorization is still required for certain services/procedures regardless of network status.
- Please refer to our Prior Authorization lists on the Conifer and MDX websites for details.
We hope that this update demonstrates our committed partnership and continued efforts to improve your ability to care for our members more easily.
Claims and Encounter Submissions
For claims and encounters with dates of service on or after January 1, 2024, please submit claims and encounter data as follows: Instructions
Payer Name:
- Conifer Health Solutions
or
- CAP Management Systems
Change Health (Optum or Emdeon)
Payer Name:
- Conifer Health Solutions
or
- CAP Management Systems
Mailing Address
Conifer Health Solutions
P.O. Box 261040
Encino, Ca 91426
Authorization Requests
For authorization requests submitted on or after January 1, 2024, please use the Conifer CapConnect provider portal, or continue to fax MDX Hawaii Prior Authorization and Specialty Referral Request Forms to
(808)532-6999. For instructions on how to register for the provider portal see below.
As of 3/1/2024, MDX HI will no longer accept electronic claims for DOS 2023 and prior. Claims for 2023 and prior need to be submitted via paper to:
MDX Hawaii
Pacific Guardian Center- Makai Tower
733 Bishop Street
Suite 3000
Honolulu, HI 96813-4016
Starting on January 1, 2024, specialty drug authorization approvals will be for a period of 3 months, and quantity may not be specified on notification.
*Note: Conifer will be honoring the 2023 MDX Prior Authorization List (PAL) requirements until a 2024 PAL becomes available. More information will be provided in the upcoming months on Cap Connect.
If you have questions, please contact Conifer Customer Service: 1-800-851-7110
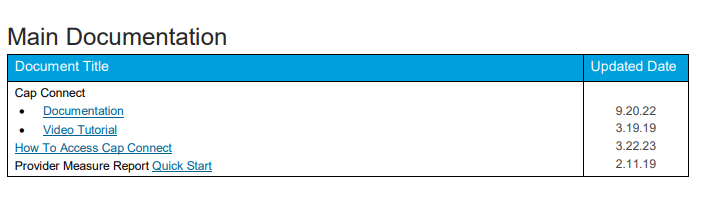
Getting started with the CapConnect provider portal, you can:
- View membership roster
- View claims status for dates of service on or after January 1, 2024
- Submit authorizations for dates of service on or after January 1, 2024
- Receive important MDX Hawaii and Conifer announcements
Conifer will activate designated usernames and initial passwords.
A powerpoint (attached below) and recorded training will be available on the Cap Connect provider portal.
Conifer Health Solutions CapConnect Presentation
Video Tutorial on Cap Connect:
First, after Log In and at Home Page – Click on User Documentation –
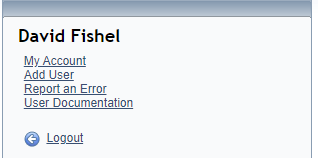
Secondly, select Video Tutorial from top section titled “Main Documentation” on page 2 of opened document